You may have been told or know someone that has been told they have stenosis, but what does that actually mean and what can be done?
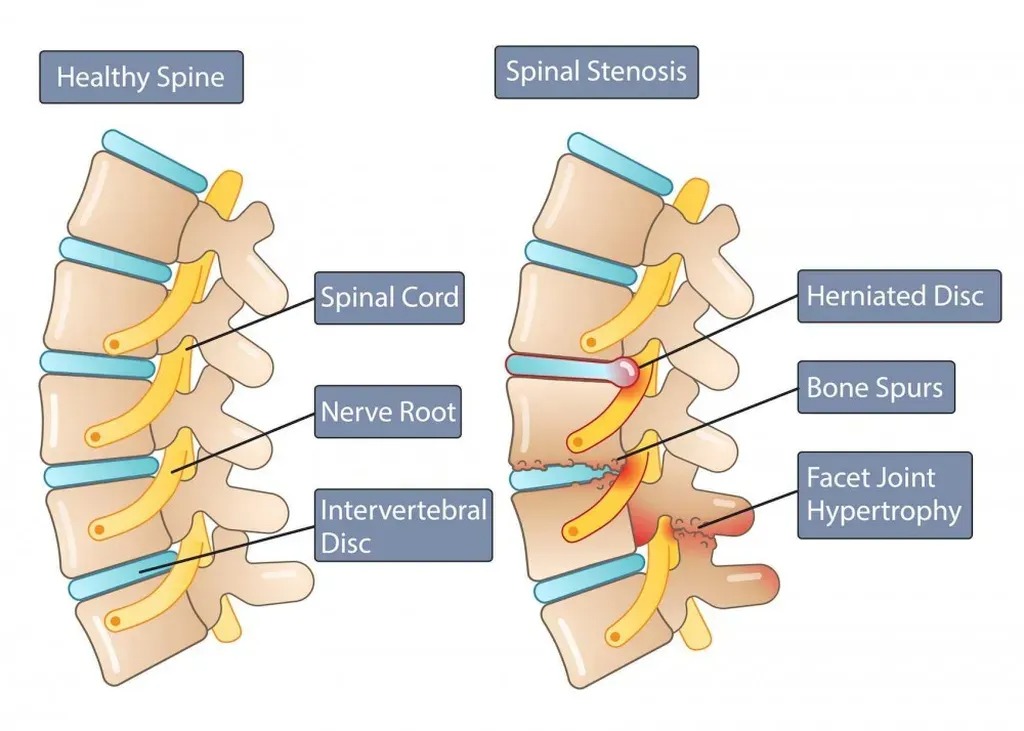
Stenosis is defined as constriction or narrowing of a passageway or opening. An example would be when a disc herniates and causes the spinal canal to become smaller in diameter. Stenosis can also be congenital (you are born with it). In congenital stenosis, there is pre-existing narrowing of the spinal canal which is a RISK FACTOR to spinal cord injury. During a traumatic event, a disc herniation in that area will have a greater detrimental effect because there is no room in the spinal canal and the injury can cause greater insult on the spinal cord or nerve roots.

Yellow arrow = disc herniation compressing spinal cord
Half of all people over 50 years of age and 75% of those over 65 years of age have a narrow cervical canal, which represents the most frequent risk factor for a cervicomedullary traumatism in the adult population. Moreover, the cervical spinal cord is particularly vulnerable because it is not thoroughly vascularized, especially in the elderly population. In some cases, the pre-existing spinal stenosis results in significant spinal cord injury resulting in complete or incomplete paralysis below the level of compression.
A “transient” compression of the spinal cord due to a congenitally narrowed spinal canal that appears normal on MRI, but has damaged the cord nonetheless. This is called neuropraxia and creates the same feeling as the one you get when your hand or foot “goes to sleep.” An article by Clark, Auguste, and Sun (2011) defines and explains cervical cord neuropraxia. The authors state, “Cervical cord neurapraxia is defined as a transient neurological deficit following cervical spinal cord trauma” (Clark et al., 2011 p.) They continue by saying, “The mechanism of injury is typically hyperextension, but cervical cord neurapraxia can occur after hyperflexion and axial loading as well” (Clark et al., 2011 p.1). They state finally, “In adults, a stenotic canal will predispose patients to cervical cord injury at the level of stenosis following an extension, flexion, or axial load injury. Therefore, surgery should be considered for a focal lesion causing cord compression” (Clark et al., 2011, p.4).

Spinal stenosis can occur in the central and lateral canals and can predispose the neural structures to injury with less trauma. In some cases, this can occur with small or no disc herniation. Clinical evaluation that details and documents these events is a critical component of care in this patient population. Proper diagnostic workup, including neurological evaluation and advanced imaging, is an important part of determining causation, bodily injury and its correlation to persistent functional loss.
Lamothe, G., Muller, F., Vital, J. M.. Goossens, D., & Barat, M. (2011). Evolution of spinal cord injuries due to cervical canal stenosis without radiographic evidence of trauma (SCIWORET): A prospective study. Annals of Physical and Rehabilitation Medicine, 54(4), 213–224.
Clark, A. J., Auguste, K. I., & Sun, P. P. (2011). Cervical spinal stenosis and sports-related cervical cord neurapraxia. Neurosurgical Focus, 31(5), E7.